Are blogs still a thing? A few months ago, while commuting to work, I started thinking about keeping a journal to serve as a processing tool for myself. I decided to brush the cobwebs off this site and hijack it to use as an outlet. Maybe others will find my experiences helpful.
Here we go…
In March of 2024, while vacationing in New York for Spring Break, my mom started complaining about heartburn. The discomfort continued after we returned home, so she went to her doctor who suggested that she start taking Pepcid AC. After return visits with no improvement, my mom was eventually referred to a gastroenterologist (GI) who prescribed acid reflex medication, advised her to eat small meals, and avoid spicy or greasy foods. After numerous visits to her GI with no relief, she was informed that she had some gallstones. Her gallbladder was removed on July 26, 2024. She still continued to experience digestive challenges. She complained that her food felt like it would get stuck in her throat and she had to drink a lot of water to force it down. Her portions were so small and the variety of food she ate became so limited she was starting to lose weight. After a scan of her esophagus, she was told it was inflamed and was prescribed pantoprazole at the beginning of August 2025. After about 2 weeks of taking the pantoprazole, she started feeling tired and noticed her abdomen swelling. She did some research online and noticed that stomach swelling was a side effect of the medication so she decided to stop taking the medicine (RECOMMENDATION: speak with the prescribing doctor about any side effects you may be having prior to stopping said medication as some medications require the patient to wean off of it to prevent more adverse side effects)
After my mom discontinues the medicine, she continues to feel discomfort. After a visit with her primary care (PCP), the PA diagnoses her with a urinary tract infection (UTI) and prescribes antibiotics. At that time, she mentions that her abdomen felt swollen. The PA noted that she had gained 6 lbs. since the last time she had been seen and it was probably just weight gain. This was a dismissive response to her concern! When she told me his response, I decided I needed to get involved. I suggested going to the Emergency Room (ER) but she wanted to see if the antibiotics would help. She finished the antibiotics and could urinate without discomfort but still felt “off” so she scheduled a follow up appointment. I told her we should just go to the ER because she should not suffer over the weekend, but she insisted to wait for her scheduled doctor appointment on Monday.
On August 25th, 2025 I experienced first hand how challenging it is to navigate the US healthcare system. I took the day off work and went with my mom to her PCP appointment. I told him that her stomach swelling was abnormal. I questioned how the rest of her could look so gaunt and her stomach be so distended. Something was wrong. We brought up our concerns about the pantoprazole medication that she stopped taking. He recommended that she take magnesium citrate to relieve possible bloating and constipation and also submitted a referral for an abdominal CT scan. (RECOMMENDATION: ask for a printout of ALL the medications each doctor has on file). The PCP was naively hopeful that we would be able to get the CT scheduled that same day. After calls to the insurance company, the imaging center, and a request for an updated referral from the PCP, the earliest date we could schedule the CT scan was Thursday, August 28. (RECOMMENDATION: if you are planning to call the insurance company on behalf of a patient, request a HIPPA form to be mailed to the patient so they can fill it out and give you authorization to speak on their behalf. Their verbal authorization is only valid for 7 days).
On Thursday, 8/28/25, I take my mom to get a CT scan and the PCP gets the results and confirms that her abdomen is filled with fluid so asks her to come in and get some bloodwork done. She is told that they will call her with the results, probably on Monday. The PCP states that if she is not in any pain and does not have fever there is no need to go to the ER.
Fri. 8/29 -Before going to work, I check on my mom and she tells me she isn’t in pain but is feeling “weird” and had to take 2 Ibuprofen every couple of hours throughout the night. She was not in pain, just extremely uncomfortable. Also, my cousin got in touch with her and shared sad news that her sister had passed away earlier in the month. My brain cannot even process that news so we put a pin in that and I order her to get dressed so I can take her to the ER. The ER performs a CT scan and runs some bloodwork. The ER doctor notes her esophagus is incredibly inflamed and she has signs of liver and/or heart failure with dangerously low sodium levels (seizure inducing). She is admitted into the hospital. The hospital performs a paracentesis and extracts out 6.7 liters of fluid from my mother’s abdomen. When she was admitted into the hospital, she weighed 124, after the procedure, her weight was 109…what in the actual…?!? My mom received a voicemail from her PCP while we are in the ER. Apparently they received the bloodwork results and noticed the low sodium and recommended that my mom go to the ER immediately (ANNOYING).
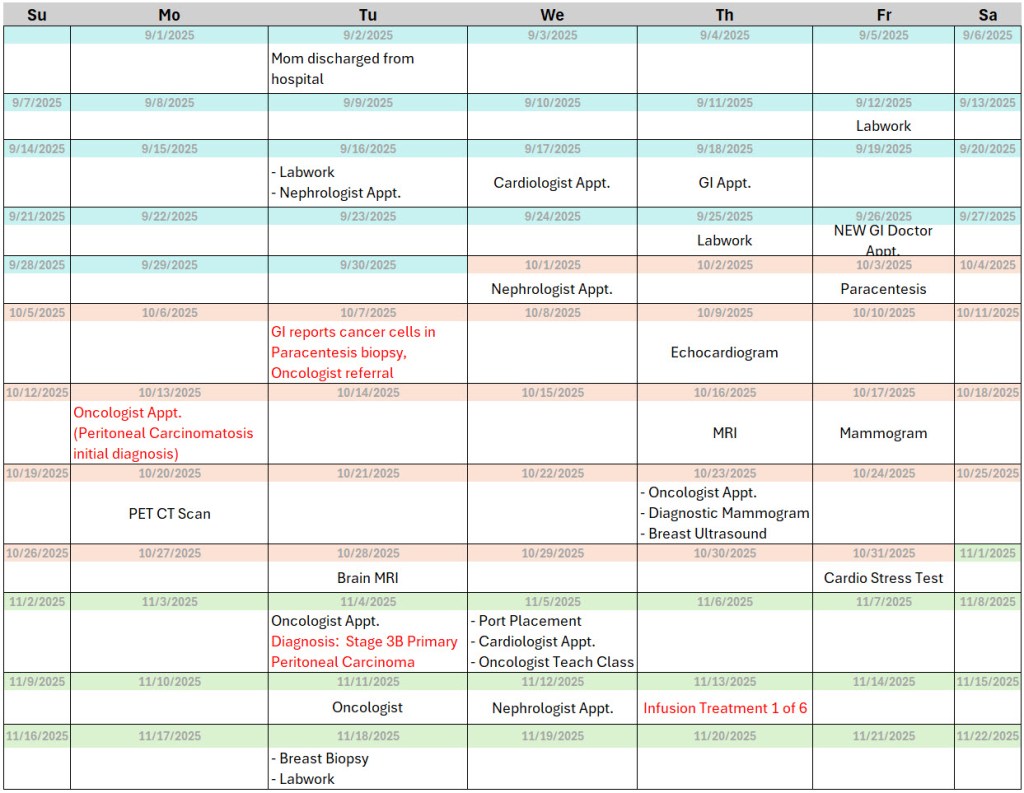
It happened to be Labor Day weekend, so things moved slow at the hospital. During her hospital stay, she is seen by two specialists: a gastroenterologist and a nephrologist. The doctors will not release her, they continue bloodwork and monitoring and schedule an endoscopy procedure on Tuesday (9/2/25). Frustratingly enough, the endoscope showed nothing concerning so the doctor discharged my mom that same day. After 5 days in the hospital, they sent us on our merry way. The staff did not even offer her a wheelchair to the car. After days of being labeled a fall risk, they just expected her to walk herself all the way downstairs to the car…how bizarre!
Her hospital discharge paper was covered with scary words: Liver Cirrhosis, Congestive Heart Failure. My mom does not drink alcohol and aside from having diabetes and high blood pressure, her heart health has never been a concern. The hospital staff stabilized my mother and now we owned the responsibility to follow up with her PCP, gastroenterologist, & nephrologist. I had to request a cardiologist referral from the PCP, because for some reason even with the congestive heart failure note, the hospital had not assigned my mom a cardiologist during her hospital stay.